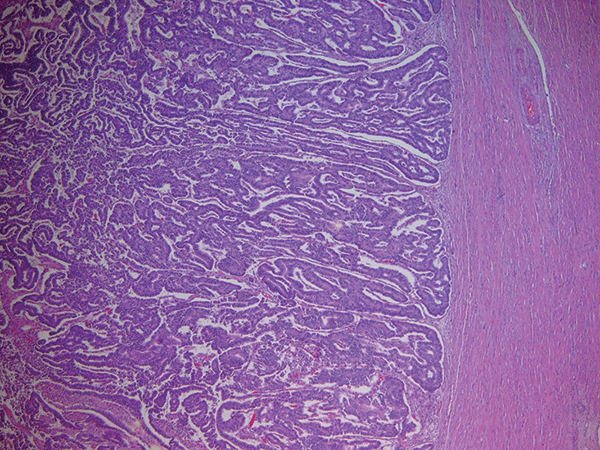
CRISPR, or Clustered Regularly Interspaced Short Palindromic Repeats, is being applied extensively in genetic engineering. Using CRISPR–associated enzyme 9 (Cas9) and guide RNA (gRNA), scientists have the ability to utilize CRISPR to easily and accurately genetically modify organisms to contain, remove, or alter a selected gene sequence. There has been promising research suggesting that, due to CRISPR’s ability to edit the genome of an organism, CRISPR could be used to treat a variety of diseases and disorders in the human body—including cancer. In fact, scientists have already used CRISPR to treat certain types of cancers, such as leukemia and lung cancer. A new study indicates that CRISPR may also be the answer to a cure for endometrial cancer, which is responsible for the deaths of nearly 8000 women annually, according to the Washington University School of Medicine in St. Louis. See also: Cancer; CRISPR/Cas9 gene editing; Enzyme; Genetic engineering; Ribonucleic acid (RNA)
The role of gRNA, which is designed to code for the desired DNA sequence, is to show the Cas9 enzyme to the targeted section of the DNA that needs to be edited. Together, gRNA and Cas9 create a plasmid—a piece of DNA that is independent of a cell’s chromosomes and can be incorporated into the cell’s genome to achieve a desired phenotype. For example, in a recent experiment, scientists used mice with endometrial cancer cells as a model organism, and the plasmid carried a CRISPR drug that has been used to treat other forms of cancer in the past. The engineered plasmid was brought to the mice’s cancer cells using a microbubble (MB), which was controlled using ultrasound. This allowed scientists to deliver the CRISPR drug directly to the cancer cells while preventing the drug from harming healthy cells in the mice. See also: Biotechnology; Deoxyribonucleic acid (DNA); Plasmid
MBs are imperative in the process of allowing the CRISPR drug to enter the cell body because the DNA of the plasmid being carried by the MB is negatively charged, but the MB itself is positively charged. Because the cell membrane is negatively charged, the positively charged MB binds to the membrane and allows the negatively charged plasmid to travel into the targeted cell, which the plasmid normally would not be able to do. Therefore, once the MB reaches a cancer cell, it attaches to the cell membrane and allows the CRISPR drug to enter the cell. See also: Cell membrane; Drug delivery system
Once inside the cancer cell, gRNA binds to the section of DNA that is targeted to be altered using a process called non-homologous end joining (NHEJ). Then, the Cas9 enzyme cuts the DNA at the chosen section, allowing the gene that is coding for the cancer-causing mutation to be silenced. When the cell detects that its DNA has been damaged, the cell attempts to repair the DNA molecule. However, as the cell begins to replicate its DNA to repair the damaged section, the cell inadvertently incorporates the gRNA genetic code into the newly created DNA. In the mouse model experiment, NHEJ stabilized and then killed the cancer cells, ceasing cell replication and stopping the spread of cancer. The success of this experiment holds promising hope for women with endometrial cancer, one of the most common gynecological cancers in women. The NHEJ method could enter human trials if results continue to show promise and the CRISPR drug delivery system increases in accuracy. See also: Animal testing; Expanded range for CRISPR gene editing; Gene silencing





