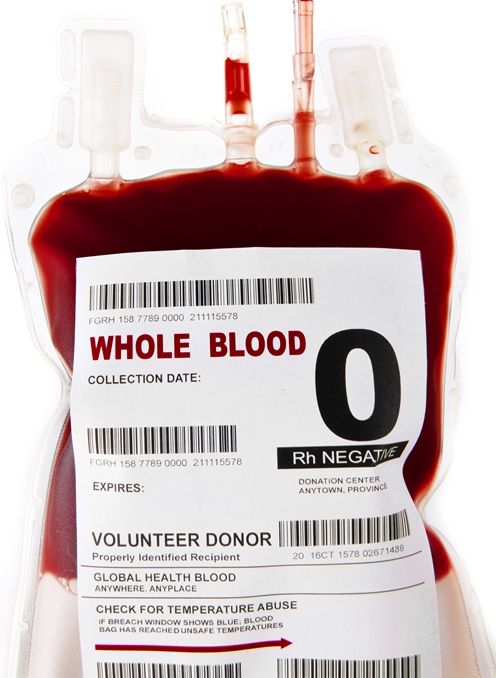
The four main blood types (blood groups) found in humans are A, B, AB, and O. Two particular antigens (A and B) determine the specific blood type—A antigen is present in type A blood; B antigen is present in type B blood; both A and B antigens are present in type AB blood; and neither A nor B antigen is present in type O blood. The latter is the most common blood type and is known as the universal donor because it can be given in a transfusion to any patient (as both A and B antigens are absent in type O). Type A is the next most-common type, followed by type B and then type AB. Because of the high demand for type O blood, especially in emergency situations when time does not allow for proper crossmatching (a laboratory test performed prior to a blood transfusion to determine whether donor blood is compatible with the recipient's blood), the certainty of a steady supply of type O blood is of paramount importance. Recently, scientists identified two enzymes in the human gut that can convert type A blood to type O. If future developments were to allow investigators to employ this enzymatic methodology in human patients in a safe and predictable way, it could potentially provide the opportunity to increase the amount of type O blood stored in blood banks by almost twofold. See also: Antibody; Antigen; Antigen-antibody reaction; Blood; Blood group; Blood group genotyping; Crossmatching; Enzyme; Immunology; Serology; Transfusion
The antigens found on the outside of red blood cells are sugar molecules. In particular, the structures of sugars found on types A and O blood are very similar, but type A has an extra N-acetylgalactosamine (GalNAc) sugar. Most importantly, the presence of this extra sugar is responsible for the immune response that occurs when, for example, type A blood is given in a transfusion to a person possessing a blood type other than type A blood. Therefore, if a method could remove the GalNAc sugar from type A blood cells, then it would essentially transform the blood into type O. Scientists analyzing a bacterium found in the microbial flora (also termed microbiota or microbiome) of the human gut (intestine) have discovered two enzymes that accomplish the steps necessary to remove the GalNAc from type A blood cells. See also: Bacteria; Bacteriology; Human microbiota; Intestine; Microbiome
The bacterium in question is known as Flavonifractor plautii. It produces two enzymes that, in tandem, enable the bacterium to consume GalNAc sugars as a food source. Scientists isolated a GalNAc deacetylase (which converts the sugar antigen to an amine, forming an intermediate structure) and a galactosaminidase (which then removes the amine) from the bacterium and observed that the enzymes could excise GalNAc sugars from type A blood cells. Even more promising is the fact that very small amounts of the enzymes were necessary to remove the type A–defining sugars and convert type A blood to type O. Thus, investigators are encouraged that this technique could work efficiently. However, the process needs to be tested thoroughly to ensure that all of the GalNAc antigens have been removed and also to verify that no other changes are made to the red blood cell surface. If the method proves to be effective, it would broaden the availability and capacity of type O blood. See also: Amine; Medicine





