Key Concepts
A fluid connective tissue that circulates in the vascular system (blood vessels) of the body. Blood circulates through the body via vascular blood vessels (arteries, veins, and capillaries). Blood consists of plasma (the fluid component) and cells floating (suspended) within it (Fig. 1). The chief components of plasma are proteins (albumin and globulins), anions (mainly chloride and bicarbonate), and cations (mainly sodium, with smaller concentrations of potassium, calcium, and magnesium). The cells are derived from extravascular sites and then enter the circulatory system. They frequently leave the blood vessels to enter the extravascular spaces, where some of them may be transformed into connective tissue cells. The fluid part of the blood is in equilibrium with the tissue fluids of the body. The circulating blood carries nutrients and oxygen to the body cells; therefore, it is an important means of maintaining the homeostasis of the body. In addition, blood carries hormones from their sites of origin throughout the body, and is thus the transmitter of the chemical integrators of the body. Blood plasma also circulates immune bodies and contains several of the components essential for the formation of blood clots. Finally, blood transports waste products to excretory organs for elimination from the body. Because of its basic composition (cells surrounded by a matrix), development, and ability to modify into other forms of connective tissues, blood can be regarded as a special form of connective tissue. See also: Blood vessel; Circulation; Connective tissue; Homeostasis; Immunology
Formed elements
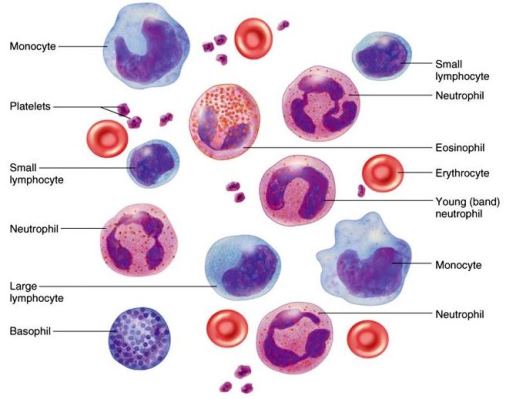
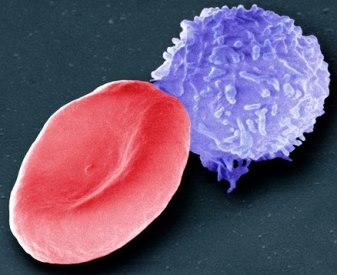
The cells of the blood include the red blood cells (erythrocytes) and the white blood cells (leukocytes) [Fig. 2]. In all vertebrates, except nearly all mammals, the red blood cells or corpuscles contain a nucleus and cytoplasm rich in hemoglobin. In contrast, in nearly all mammals, the nucleus has been extruded during the developmental stages. Importantly, there are genetically determined markers on the surface of the cellular blood elements; these markers determine the various blood types or groups. See also: Blood group
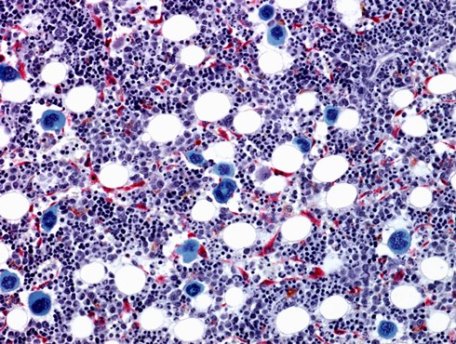
Hematopoiesis is the process by which the cellular elements of the blood are formed. Some of the blood cells are terminal cells, in the sense that they are fully differentiated and have little or no capacity for division. These include the erythrocytes and the granulocytes. The agranular leukocytes may develop extravascularly into other cell types (macrophages, fibroblasts, or plasma cells). All blood cells are formed in the hematopoietic organs (chiefly lymph nodes and spleen for agranular leukocytes, and bone marrow for erythrocytes, platelets, and granular leukocytes). See also: Hematopoiesis
Although blood cells occur in all vertebrates, they differ in density, relative proportions, morphology (to some extent), and their sites of origin. For example, the red blood cells of fish are nucleated, are ovoid or spindle-shaped, and may be larger than in any other vertebrate. They are also large in frogs, where they are somewhat less oval than in birds. There also are notable differences in the internal structure of the leukocytes, especially with regard to the size, shape, and staining properties of the granular leukocytes.
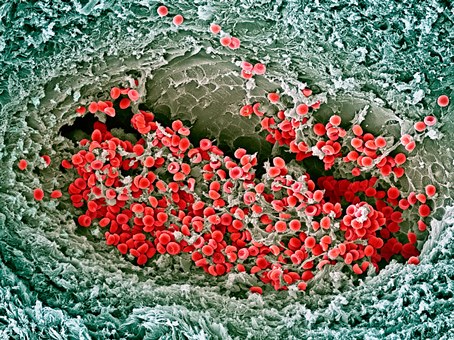
Erythrocytes
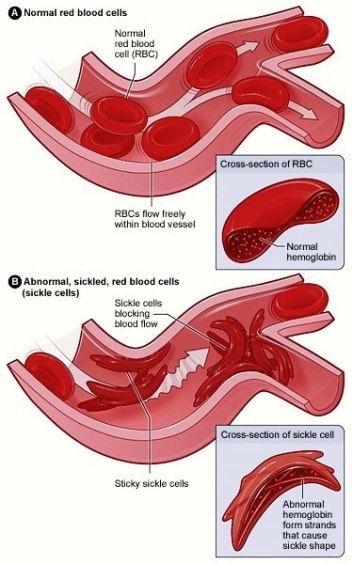
In normal adult men and women, the blood contains approximately 5,000,000 and 4,500,000 erythrocytes per cubic mm, respectively. Human erythrocytes measure about 8 μm in diameter and about 2 μm at their thickest, and they have a biconcave shape. They contain hemoglobin, which imparts to them their color, and possess an envelope, which appears highly structured when viewed with an electron microscope. The hemoglobin is involved in the transport of oxygen and carbon dioxide, and it plays a role in maintaining a constant pH in the blood. When circulating in the blood vessels, the red blood cells are not evenly dispersed. In the narrowest vessels (the capillaries), the erythrocytes are often distorted. In certain conditions, they may be densely aggregated; this is known as a sludge. The erythrocytes respond to changes in osmotic pressure of the surrounding fluid by swelling in hypotonic fluids and by shrinking irregularly in hypertonic fluids. Shrunken red blood cells are referred to as crenated cells. The average life of a mature red blood cell is surprisingly long, spanning about 120 days. Sickle cell disease is an inherited disorder that causes erythrocytes to assume a sickle shape, impairing their function (Fig. 3). See also: Hematologic disorders; Hemoglobin; Sickle cell disease
Leukocytes
In humans, the white blood cells in the blood are fewer in number, amounting to about 5000–9000 per cubic mm. In general, there are two varieties: agranular and granular leukocytes. The agranular cells include the small, medium, and large lymphocytes and the monocytes. The small lymphocytes are spherical, measuring about the diameter of erythrocytes or a little larger, and constitute about 20–25% of the white blood cells. The medium and large lymphocytes are relatively scarce. In all lymphocytes, the nucleus occupies nearly the whole volume of the cell, and the cytoplasm (which surrounds it) forms a thin shell. The typical monocyte is commonly as large as a large lymphocyte (12 μm), constituting 3–8% of the white blood cells. The nucleus is relatively small, eccentric, and oval or kidney-shaped; the cytoplasm is relatively larger in volume than that in lymphocytes.
The granular white blood cells or granular leukocytes comprise three varieties: neutrophils, eosinophils, and basophils. Neutrophils are large granular leukocytes with cytoplasmic granules that stain best with neutral dyes. Eosinophils are granular leukocytes having cytoplasmic granules that stain with acid dyes (most commonly, eosin dyes). Basophils are white blood cells with granules that stain with basic dyes and are water-soluble. The structures of neutrophils, eosinophils, and basophils vary somewhat in different species. In humans, the neutrophils make up 65–75% of the leukocytes. They are about as large as monocytes, with a highly variable nucleus. The cytoplasm contains numerous minute granules. In certain conditions, the neutrophils leave the blood vessels and wander into the connective tissue ground substance, where they may then disintegrate, releasing their granules. These granules are rich in certain hydrolytic enzymes, which become active and take part in some phases of the defense mechanisms of the body. The granules are considered to be pure lysosomes, which are released from the cell during inflammation and in other conditions. Human eosinophils (also called acidophils) are about the same size as the neutrophils, but they are less numerous, constituting about 1% of the leukocytes. The granules that fill the cytoplasm are larger than those of the neutrophils. The basophils found in humans are about the same size as the other granular leukocytes. The nucleus may appear elongated or with one or more constrictions. See also: Enzyme; Lysosome
The functions of the leukocytes while they are circulating in the blood are not known. However, when they leave the blood vessels and enter the connective tissue, they constitute an important part of the body's defense and repair mechanisms. Many of the cells are actively phagocytic and engulf debris and bacteria. Lymphocytes are of two major kinds: T cells and B cells. They are involved in the formation of antibodies and in cellular immunity. Lymphocytes develop into plasma cells, which form antibodies even more effectively than lymphocytes. In addition, lymphocytes and monocytes may develop extravascularly into macrophages (which are also phagocytic) and subsequently into fibroblasts. The fibroblasts are important in the formation of new connective tissue in regions of injury. See also: Antibiotic; Cellular immunology; Fibroblasts; Macrophages; Phagocytosis
Platelets
Blood platelets are small spindle-shaped or rodlike bodies that measure about 3 μm in length. They occur in large numbers in circulating blood. In suitably stained specimens, they consist of a granular central portion (chromomere) embedded in a homogeneous matrix (hyalomere). They change their shape rapidly on contact with injured vessels or foreign surfaces and take part in clot formation. During this process, numerous fibrils of fibrin radiate from the platelets. The platelets are not to be regarded as cells and are thought to be cytoplasmic bits broken off from their cells of origin in the bone marrow—the megakaryocytes (Fig. 4).
Plasma
Plasma is the residual fluid of blood left after removal of the cellular elements. Serum is the fluid that is obtained after blood has been allowed to clot and the clot has been removed. Serum and plasma differ only in their content of fibrinogen and several minor components (which are, in large part, removed in the clotting process). See also: Fibrinogen
The major constituents of plasma and serum are proteins. The total protein concentration of human serum is approximately 7 g/ml, and most other mammals show similar levels. Birds, reptiles, amphibians, and most fishes have lower protein concentrations of approximately 3–5 g/100 ml. It has been demonstrated that serum protein is a heterogeneous mixture of a large number of constituents. More than 60 protein components have been identified and characterized. See also: Protein
Albumin
Albumin makes up more than one-half of the total plasma proteins and has a molecular weight of 69,000 daltons. Because of its relatively small molecular size and its high concentration, albumin contributes to 75–80% of the colloid osmotic pressure of plasma. Therefore, it plays a major role in the regulation of the intravascular volume and the fluid exchange between the vascular system and the extravascular space. In addition, albumin serves as a transport protein for various substances, including small ions (for example, calcium and iodine) and organic compounds (for example, bilirubin). See also: Albumin
Immunoglobulins
The immunoglobulins, which represent approximately one-sixth of the total protein content, largely constitute the gamma-globulin fraction. The immunoglobulins are antibodies circulating in the blood and thus are also called humoral antibodies. They are of great importance in an organism's defense against infectious agents and other foreign substances. Of the different classes of immunoglobulins that can be distinguished, the principal ones are IgG, IgM, IgA, IgD, and IgE. Antibodies are formed under the stimulus of a foreign substance, the antigen, and are specifically directed against this antigen. The specificity of an antibody reaction appears to be ensured by a specific molecular structure in certain parts of the antibody molecule. See also: Immunoglobulin
Other proteins
The lipoproteins comprise another class of serum proteins and make up slightly less than 10% of the total. Presumably, they serve as transport proteins for lipids, including cholesterol, cholesterol esters, and phospholipids. Other serum proteins that function as carriers for specific substances are transport proteins for metal ions (for example, the iron-binding protein, transferrin, and the copper-binding protein, ceruloplasmin). Several serum proteins have the capacity to inhibit proteolytic enzymes, thereby protecting serum and possibly tissue proteins against enzymatic degradation. Also present in appreciable concentrations are several other glycoproteins, numerous enzymes, and an array of clotting factors.
The complement components constitute another key group. Complement is an important effector system in immune reactions, with the target being the cell surface membranes. Its action may result in cell lysis, directed migration of cells, and preparation of damaged cells for uptake and removal by other cells (via phagocytosis). See also: Complement
Other constituents
In addition to the proteins, many other important classes of compounds circulate in the blood plasma. Most of these are smaller molecules that diffuse freely through cell membranes; therefore, they are more similarly distributed throughout all the fluids of the body and are not as characteristic for plasma or serum as the proteins. In terms of their concentration and their function, the electrolytes are most important. They are the primary factors in the regulation of the osmotic pressure of plasma, and they contribute also to pH control. The chief cations are sodium, potassium, calcium, and magnesium. The chief anions are chloride, bicarbonate, phosphate, sulfate, and organic acids. See also: pH regulation (biology)
Glucose is also an important constituent of plasma because it is a major source of energy for cells throughout the body. In addition, free amino acids, the constituents of peptides and proteins, circulate in plasma. See also: Amino acid; Glucose
Blood coagulation
When mammalian blood is shed, it congeals rapidly into a gelatinous clot of enmeshed fibrin threads that trap blood cells and serum (Fig. 5). Modern hematology indicates a succession of reactions leading to the formation of insoluble fibrin from a soluble precursor, fibrinogen (factor I).
Thrombin
The agent ultimately responsible for the formation of fibrin is a proteolytic enzyme, thrombin, which splits four small polypeptide fragments (the fibrinopeptides) from each molecule of fibrinogen. The remainder of the fibrinogen molecule, now called the fibrin monomer, polymerizes to form insoluble fibrin, that is, the structure of the clot. The strands of fibrin are given added strength through covalent bonds between adjacent fibrin monomers. It should be noted that thrombin does not exist as such in circulating blood, but is generated during clotting from an inactive precursor, prothrombin (factor II). Interestingly, the coagulation of blood can be induced by certain snake venoms, which either promote the formation of thrombin or clot fibrinogen directly, accounting in part for their toxicity. Bacterial enzymes, including staphylocoagulase (derived from Staphylococcus aureus), may also induce clotting. See also: Toxin
Platelets
Besides furnishing phospholipids for the clotting process, platelets help to stanch the flow of blood from injured blood vessels by accumulating at the point of injury, forming a plug. Platelets participate in the phenomenon of clot retraction, in which the blood clot shrinks, expelling liquid serum. Although the function of retraction is unknown, individuals in whom this process is impaired have a bleeding tendency.
Hereditary defects
Hereditary deficiencies of the function of the various protein-clotting factors have been described, including classic hemophilia (in which antihemophilic factor is present in a nonfunctional form). Most of the hereditary functional deficiencies are associated with a bleeding tendency. Therapy for bleeding due to deficiencies of clotting factors often includes the transfusion of blood plasma or fractions of plasma rich in particular substances that the individual may lack. See also: Hemophilia; Human genetics; Transfusion
Heparin
Heparin, a polysaccharide–sulfuric acid complex found particularly in the liver and lungs, impairs coagulation by interfering with the formation of the prothrombin-converting principle and with the action of thrombin. Both coumarin and heparin are used clinically to impede coagulation in thrombotic states, including thrombophlebitis and coronary heart disease. See also: Heparin; Thrombosis





