Key Concepts
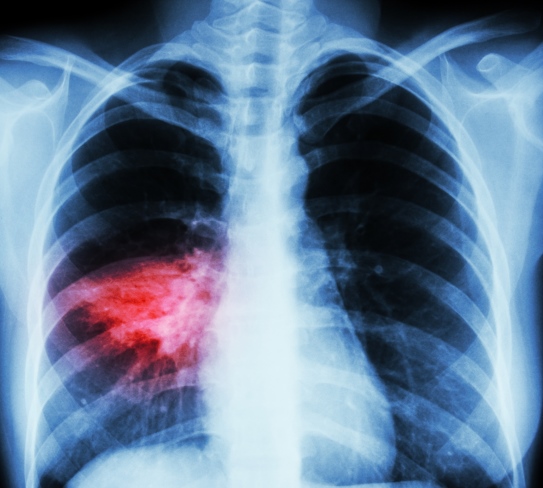
An acute or chronic inflammatory disease of the lungs. Pneumonia (Fig. 1) is a serious inflammatory lung disorder that can affect one or both of the lungs. It is caused by numerous microbial, immunological, physical, or chemical agents, and it is associated with exudate in the lumens (inner spaces) of the lung's alveoli (tiny air sacs). More specifically, when the lung inflammation is caused by an infectious agent, the condition is called pneumonia; in contrast, when the inflammatory process in the lung is not related to an infectious organism, it is usually called pneumonitis. See also: Inflammation; Lung; Respiratory system disorders
Pneumonia is a common immediate cause of death in persons with a variety of underlying diseases. With the use of immunosuppressive and chemotherapeutic agents for treating transplant and cancer patients, pneumonia caused by infectious agents that usually do not cause infections in healthy persons (that is, pneumonia as an opportunistic infection) has become commonplace. Moreover, individuals with acquired immune deficiency syndrome (AIDS) usually die from an opportunistic infection, such as pneumocystis pneumonia or cytomegalovirus pneumonia. Concurrent with the variable and expanding etiology of pneumonia and the more frequent occurrence of opportunistic infections is the development of new antibiotics and other drugs used in the treatment of pneumonia. See also: Acquired immune deficiency syndrome (AIDS); Antibiotic; Chemotherapy and other antineoplastic drug treatments; Cytomegalovirus infection; Immunological deficiency; Opportunistic infections; Transplantation biology
Infectious pneumonia
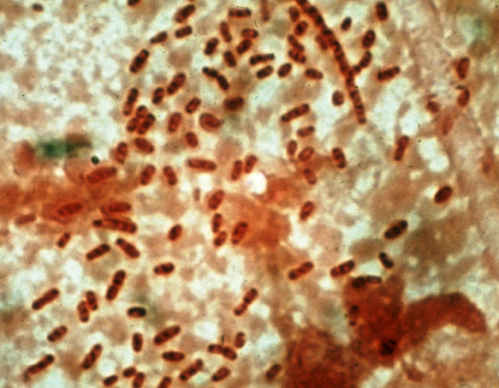
Bacteria, as a group, are the most common cause of infectious pneumonia. Common bacterial agents causing pneumonia are Streptococcus pneumoniae, other species of Streptococcus, Staphylococcus species, Haemophilus influenzae, Klebsiella species (Fig. 2), Pseudomonas aeruginosa, Legionella pneumophila, Mycobacterium tuberculosis, and Mycoplasma pneumoniae. Some of these bacteria are normal inhabitants of the body and proliferate to cause disease only under certain conditions. Other bacteria are contaminants of food or water. See also: Mycobacterial diseases; Streptococcus pneumoniae (pneumococcus)
Most bacteria cause one of two main morphologic forms of inflammation in the lung. Streptococcus pneumoniae causes a type of pneumonia referred to as lobar pneumonia, in which an entire lobe of a lung or a large portion of a lobe, usually the lower lobe, becomes consolidated (firm and dense) and nonfunctional secondary to an influx of fluid and acute inflammatory cells (polymorphonuclear leukocytes) that represent a reaction to the bacteria. This type of pneumonia is uncommon today, usually occurring in people who have poor hygiene and are debilitated. If lobar pneumonia is treated adequately, the inflammatory process may entirely disappear. However, in some instances, it undergoes a process called organization, in which the inflammatory tissue changes into fibrous tissue. This results in a permanent obliteration of the normal lung architecture, usually rendering that portion of the lung nonfunctional.
The other morphologic form of pneumonia, which is caused by the majority of bacteria, is called bronchopneumonia. In this form, there is patchy consolidation of lung tissue (Fig. 1), usually around the small bronchi and bronchioles, and most frequent in the lower lobes. This type of pneumonia may also undergo complete resolution if there is adequate treatment, although rarely it organizes.
Legionella pneumonia, often called Legionnaires' disease or legionellosis, is caused by bacteria of the genus Legionella. The condition is not uncommon, and two clinical syndromes are manifested: an acute pneumonia with a high mortality rate, and a self-limited flulike illness. Legionella pneumonia may also occur in compromised hosts as an opportunistic infection. See also: Legionnaires' disease
Viral pneumonia is usually a diffuse process throughout the lung and produces a different type of inflammatory reaction than is seen in bronchopneumonia or lobar pneumonia. Viruses that are known to cause pneumonia include influenza A, influenza B, adenovirus, respiratory syncytial virus, cytomegalovirus, and herpes simplex virus. See also: Virus
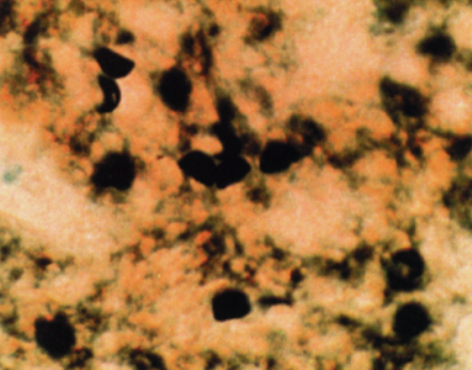
Pneumonia also can be caused by a variety of fungal organisms, especially in debilitated persons (for example, those with cancer or AIDS). In particular, pneumocystis pneumonia (Fig. 3) is caused by Pneumocystis jirovecii (also known as Pneumocystis carinii) and has been recognized as a primary cause of death in immunocompromised patients with AIDS. See also: Fungi
Hypersensitivity pneumonitis
Some persons are allergic to certain organic antigens, including the spores of various types of bacteria. When these antigens are inhaled into the lungs of susceptible persons, an inflammatory reaction occurs that can progress from acute to a more chronic disease. The most frequently recognized hypersensitivity pneumonitis is called farmer's lung: susceptible farmers or other persons dealing with such items as moldy hay inhale the spores of thermophilic actinomycetes bacteria. About 4–6 h later, they develop fever, cough, shortness of breath, and chest pain, and an x-ray shows a patchy infiltrate in their lungs. The disease can rapidly clear when the person is removed from the offending antigen or is treated with cortisone-type medicines. See also: Allergy; Antigen
Drug-induced pneumonitis
Many drugs can induce inflammation in the lungs. The mechanisms by which various drugs cause pneumonitis can either depend on the dose or be secondary to a hypersensitivity reaction. Alkylating agents (for example, busulfan, which is used in treating various types of solid tumors) are the drugs most frequently recognized to cause pneumonitis. The pneumonitis may occur weeks to months after the drug has been started and usually appears to depend on the dose. Gold sodium thiomalate (a drug used to treat rheumatoid arthritis) and amiodarone (a drug used in treating heartbeat irregularities) are agents that can cause a hypersensitivity pneumonitis that may progress to fibrosis.
Cocaine and its derivatives have been associated with the development of a nonspecific type of pneumonitis and fibrosis, as well as pulmonary hemorrhage. The exact mechanism by which cocaine causes these changes is uncertain, but it may be related to the effect of cocaine on the contraction and relaxation of blood vessels. See also: Cocaine
Other types of pneumonitis and agents
Idiopathic interstitial pneumonitis, also referred to as idiopathic pulmonary fibrosis, is characterized by a chronic inflammation in the lung in association with the formation of fibrous tissue. The cause of most cases is uncertain, although some cases have been associated with systemic lupus erythematosus. Bronchiolitis obliterans organizing pneumonitis is characterized by inflammation of the bronchioles as well as lobar fibrosis. It usually is associated with cough, fever, and chest pain. Its cause is usually unknown, and most cases are reversible when treated with cortisone-type drugs. See also: Bronchiolitis obliterans organizing pneumonia (BOOP)
Oxygen, when delivered at concentrations greater than 40% for more than 24 h, can cause inflammation in the lung. This usually begins as acute damage to the alveoli and can progress to pulmonary fibrosis. Radiation, used in the treatment of thoracic tumors, can also cause inflammation of the lung with subsequent fibrosis. Aspiration of blood or gastric contents can produce a localized region of severe inflammation and cellular death in the lung. The aspiration of an oily substance, including oily nose drops, can result in the accumulation of lipid material in the lung, referred to as lipoid pneumonitis.
Signs, symptoms, and diagnosis
The signs and symptoms of pneumonia and pneumonitis are usually nonspecific, consisting of fever, chills, shortness of breath, and chest pain. Fever and chills are more frequently associated with infectious pneumonias, but they also may be seen in pneumonitis. The physical examination of a person with pneumonia or pneumonitis may reveal abnormal lung sounds indicative of regions of consolidation of lung tissue. A chest x-ray also shows the consolidation (Fig. 1), which appears as an area of increased opacity. Cultures of sputum or bronchial secretions may identify an infectious organism capable of causing the pneumonia. In AIDS patients, fluid is frequently instilled into the pulmonary bronchial tree and then rapidly removed; examination of special preparations of this fluid may show microorganisms such as Pneumocystis jirovecii. In some cases of pneumonia or pneumonitis in which no definite cause can be determined from routine studies, the chest cavity must be opened surgically and the lung biopsied. See also: X-rays
Treatment
The treatment of pneumonia and pneumonitis depends on the cause. Bacterial pneumonias are treated with antimicrobial agents, including penicillin. If the organisms can be cultured, the sensitivity of the organism to a specific antibiotic can be determined. Viral pneumonias are difficult to treat because most drugs only help control the symptoms. The treatment of pneumonitis depends on identifying its cause; many cases are treated with cortisone-type medicines. See also: Penicillin





