Since the start of the COVID-19 (coronavirus disease 2019) pandemic, doctors and epidemiologists have identified a number of underlying medical conditions that are significantly correlated with severe illness from COVID-19. One such notable associated medical condition is obesity. Obesity, which has been classified as a disease since 2014 by the American Medical Association (the largest physician organization in the United States), is an excessive accumulation of adipose tissue (body fat) that typically leads to a variety of health risks. An individual is considered to be obese if they have a body mass index (BMI) of 30 or greater. BMI, which is used as an indicator of high body fatness, is calculated by dividing a person's weight in kilograms by the square of that person's height in meters. Using data compiled globally from almost 400,000 COVID-19 patients, investigators found that obese people who contracted COVID-19 were 113% more likely to require hospitalization, compared to people with a healthy BMI; 74% were more probable to be admitted to an intensive care unit (ICU); and 48% were more prone to dying. In addition to the correlation between obesity and COVID-19, analyses of COVID-19 patient data indicate that people who are simply overweight (having a BMI of 25–29.9) also have a higher risk of contracting severe cases of COVID-19 compared to healthy-BMI individuals. See also: Adipose tissue; Coronavirus; Critical care medicine; Disease; Epidemic; Infectious disease; Novel coronavirus is declared a global pandemic; Obesity; Virus
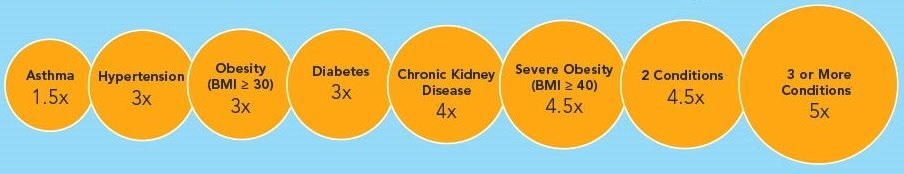
According to the World Health Organization, the global incidence of obesity has increased nearly threefold since the 1970s. Today, approximately 2 billion people worldwide are overweight, with about 650 million being obese. Because obesity has a detrimental impact on immune function and lessens host defense against viral (and other) pathogens, researchers were not surprised when COVID-19 patient data indicated a strong link between obesity and COVID-19 illness. In fact, obesity was similarly noted to be an independent risk factor for illness in a number of previous viral pandemics [for example, the 2009 H1N1 influenza (swine flu) pandemic], with severe obesity (BMI ≥ 40) being particularly associated with greater numbers of patient hospitalizations (including more ICU admissions) and deaths. As such, investigators assess people with obesity (especially severe obesity) to be distinctly at risk for infection from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; that is, the virus responsible for COVID-19). See also: Epidemic of obesity; H1N1 influenza; Immunology; Pathogen
Obesity hinders good health and is a major public health problem. Obese individuals have impaired immunity, chronic inflammation, and high blood pressure (hypertension), and their blood tends to clot more readily. In particular, adipose cells in obese people invade the spleen, bone marrow, and thymus (the body organs where immune cells are manufactured and accumulate), reducing the effectiveness of the immune system. Thus, obese individuals are more vulnerable to COVID-19. In the United States, about 40% of the adult population is considered obese. As such, obesity is likely a contributing factor toward why the death rate in the United States is the highest in the world. In a survey conducted in August 2020 in the United States, approximately 77% of 17,000 individuals hospitalized with COVID-19 were overweight (29%) or obese (48%). A similar study of COVID-19 patients hospitalized in England found similar results. See also: Epidemiology; Hypertension; Immunity; Inflammation; Public health
COVID-19 also affects certain population groups more than others. In particular, African Americans, Native Americans, and Latino groups in the United States have been affected disproportionately by COVID-19. For example, black people are more than 3.5 times more likely to die of COVID-19 compared to white people. Investigators surmise that obesity is possibly a contributing reason for this unbalanced toll of cases in population groups reporting high rates of severe COVID-19. Furthermore, obese individuals frequently delay or avoid medical care, often as a result of fear of stigmatization, thereby heightening the prospect of serious illness or fatality. Therefore, it is imperative that clinical trials of potential COVID-19 pharmacotherapeutics and vaccines include individuals with high BMIs. Without inclusion and collection of such data derived from obese individuals, a full understanding of the relationship between obesity and COVID-19 will remain inadequate.
Because of the risk with regard to COVID-19, obese individuals need extra vigilance. Daily exercise and weight loss are two important ways to boost overall metabolic function and health of an obese person and decrease the likelihood or severity of COVID-19 illness.





