Key Concepts
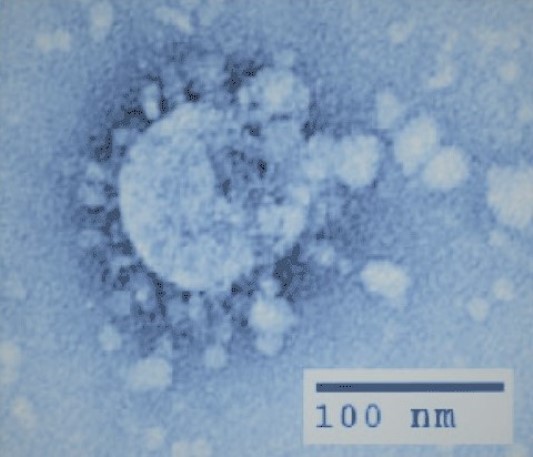
A viral respiratory illness, often life-threatening, caused by a strain of the SARS coronavirus. Severe acute respiratory syndrome (SARS) is a serious viral respiratory disease caused by the severe acute respiratory syndrome coronavirus (SARS-CoV) [see illustration]. SARS was first recognized in November 2002. An international outbreak involving 26 countries, 8098 cases, and 774 deaths subsequently developed, ending in July 2003. Since then, two isolated cases of SARS and one cluster of 11 cases (including one death) have been identified, resulting from the "escape" of SARS-associated coronavirus from research laboratories. In addition, four isolated cases of SARS with no secondary cases were identified in December 2003 and January 2004. Aside from these scenarios, there has been no evidence of any reemergence of SARS, and no cases of SARS have been identified since 2004. Regardless, much interest and research continues into better understanding SARS in order to be prepared for its possible reemergence and/or the emergence of other similar pathogens. The global pandemic COVID-19 (an acronym for coronavirus disease 2019) is caused by a coronavirus strain related to SARS-CoV; this novel coronavirus has been designated as SARS-CoV-2. See also: Animal virus; Coronavirus; Epidemic; Novel coronavirus is declared a global pandemic; Respiratory system disorders; Virus; Virus classification
Etiologic agent
With unprecedented speed after the recognition of SARS, a newly identified coronavirus, that is, SARS-CoV, was pinpointed as the causal agent of the disease. Coronaviruses are enveloped, single-stranded ribonucleic acid (RNA) viruses that cause a variety of diseases in animals. Prior to the discovery of SARS-CoV, only two coronaviruses were recognized as causing human disease—coronaviruses OC43 and 229E; these two viruses are associated with the common cold. In general, coronaviruses can be divided into three groups based on their genetic and protein content. However, SARS-CoV does not readily fit into any of these three groups and has been placed into a fourth group.
Data suggest that SARS-CoV evolved from animal SARS-like viruses that are closely related to SARS-CoV. SARS-like viruses have been identified in a number of different animals, including Himalayan palm civets found in food markets and eaten as a delicacy in China. Genotypic evidence suggests that cases early in the outbreak were infected with viruses more closely resembling animal SARS-like viruses than SARS-CoV and that SARS-CoV evolved from positive selective pressure acting on animal SARS-like viruses, ultimately culminating in the emergence of the predominant SARS-CoV genotype responsible for the 2002–2003 outbreak. See also: Civet
There is evidence to suggest that animal SARS-like viruses existed and were transmitted to humans, remaining clinically undetected, at least 2 years predating the 2002–2003 outbreak. However, human infection due to animal SARS-like viruses is milder and associated with less human-to-human transmission than infection with SARS-CoV. See also: Infectious disease
Epidemiology
Whether or not SARS will reemerge as it did in the 2002–2003 outbreak is debatable. The only known reservoirs of SARS-CoV are laboratories in which live SARS-CoV is being handled. Although animal reservoirs of animal SARS-like viruses exist, human or animal reservoirs of SARS-CoV have not been found. Thus, the only likely ways for SARS to reemerge are for the circumstances that permitted the selection and purification of SARS-CoV from animal SARS-like viruses to be repeated or for laboratory accidents exposing workers to SARS-CoV to occur. The risk of the former is difficult to predict until more is understood about the circumstances that permitted the selection of SARS-CoV to have occurred in the first case. The risk of the latter will be reduced by continued vigilance and reinforcement of the importance of appropriate biosafety standards to be used in laboratories in which research with SARS-CoV is being conducted. See also: Epidemiology
Transmission
SARS-CoV is typically transmitted by direct contact with people with SARS or by mucous membrane exposure to respiratory droplets from infected people. Some evidence suggests that airborne transmission or transmission via fomites (inanimate contaminated objects) may occur, but only very rarely. Transmission appears not to occur before the onset of symptoms, and it is most common from severely ill people in the second week of illness. In the 2002–2003 outbreak, transmission was almost entirely limited to households, hospitals, and immediate prehospital care.
Pathogenesis
The mechanisms by which SARS-CoV causes disease have been investigated. Angiotensin-converting enzyme 2, predominantly found in heart and kidney tissues, has been identified as a cellular receptor for SARS-CoV. However, given that SARS-CoV is found in highest numbers in lung and gastrointestinal tissue, other unidentified receptors likely also play a role. Based on clinical, epidemiologic, and virologic data, it appears that SARS-CoV, after entry via the respiratory system, is first associated with viremia (presence of viral particles in the blood), followed by predominant replication in the lung and gastrointestinal tract. However, dissemination to other organs and replication in other organs likely also occur, given that SARS-CoV RNA has been found in a wide range of organs at autopsy. Viral replication is thought to be maximal during the second week of symptoms because this is the time when SARS-CoV can be most readily detected in tissues and most efficiently transmitted to others. It has been postulated that the immune response to SARS-CoV replication in the lung is primarily responsible for the worsening of respiratory symptoms seen in some patients, typically during the third week of illness. The associated lymphopenia (a reduction of lymphocytes in the circulating blood) observed in many patients suggests that lymphocytes play a role in fighting the infection or in being infected themselves. Further study is needed to better understand the pathogenesis of and immune response to SARS.
Clinical manifestations
Patients infected with SARS-CoV may be asymptomatic, may have only mild nonspecific symptoms that do not progress, or may develop typical SARS. Patients with typical SARS usually present nonspecific symptoms at two to ten days following exposure. These symptoms include fever, myalgia (muscle pain), headache, malaise, and chills. Three to five days later, these patients develop a nonproductive (dry) cough and dyspnea (difficult or labored breathing), with approximately 25% developing watery diarrhea. Approximately 20% of patients subsequently develop worsening respiratory distress, requiring admission to an intensive care unit. Overall, 15% of patients require tracheal intubation (insertion of a tube into the trachea to maintain an airway and permit suction of the respiratory tract) and mechanical ventilation support. Approximately 10% of all patients die from progressive respiratory distress or complications of their hospital admission, typically during the third or fourth week of symptomatic illness.
Typical laboratory abnormalities at the time of presentation include a normal total white blood cell count, lymphopenia, and increased levels of two enzymes—lactate dehydrogenase and creatinine kinase (most likely due to associated lung tissue injury). However, such laboratory abnormalities are not uncommon in patients with community-acquired pneumonia due to causes other than SARS-CoV, so an accurate diagnosis of SARS cannot be made based on clinical or laboratory features alone. Approximately 75% of patients present with infiltrates on a chest radiograph (that is, the appearance of ill-defined opacities on a chest x-ray), but virtually all infected patients will eventually develop chest infiltrates, usually in the second week of illness. Multifocal infiltrates (opacities in more than one lung zone) with ground-glass appearance are more common in SARS than bacterial pneumonia. High-resolution computerized tomography may detect ground-glass opacities not detected by standard radiography. Both laboratory abnormalities and infiltrates usually progress after admission and peak at, or just after, the end of the second week of disease. See also: Pneumonia
Increased age, comorbidity (having a concurrent, but unrelated, disease), elevated levels of lactate dehydrogenase, and elevated neutrophil (large granular white blood cell) counts at the time of presentation have been associated with an increased risk of death; the case fatality rate in persons over the age of 60 approaches 50%. Infants and children appear to be protected against acquiring the infection and typically have a milder course; associated rhinorrhea (mucous discharge from the nose) is seen in 50% of those who develop symptoms.
Diagnosis
Multiple assays for the diagnosis of SARS have been developed. Reverse transcription–polymerase chain reaction (RT-PCR), which detects SARS-CoV RNA in specimens of blood, stool, and respiratory secretions taken from patients, and serologic tests, which detect SARS-CoV antibodies in the serum produced after infection, have become the mainstay of laboratory diagnosis. Viral culture appears to be less sensitive. See also: Antibody; Polymerase chain reaction (PCR); Serology
Seroconversion (development of antibodies to a particular antigen) occurs in patients with SARS from 1 to 4 weeks after symptom onset. Most patients do not develop either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies until the third or fourth week of illness. See also: Immunoglobulin
Treatment
During the 2002–2003 outbreak, many antiviral agents, such as ribavirin and lopinavir/ritonavir (which inhibit viral replication), and immunomodulatory drugs, such as interferon, steroids, and intravenous immunoglobulin (which can modify the immune response to an infection), were used in varying doses and combinations in different regions of the world. Essentially, all of these treatments reported some associated anecdotal clinical improvement. However, no definitive conclusions regarding the efficacy of any of these treatments can be made.
Many other treatments have shown promise in animal or in-vitro models. These include antiviral agents specifically directed against viral entry into cells and agents directed against expression of viral genes. Further in-vitro and in-vivo studies are needed to better determine the potential role of each of these agents as prophylaxis or treatment for SARS.
Prevention
Many candidate SARS vaccines are being developed. Preliminary work based on the immunization of animals has shown the ability of certain potential vaccines to induce immune responses to SARS-CoV. However, until effective vaccines are available for human use, the key components to prevention include early identification of cases and rapid implementation of control measures, including isolation, contact tracing, and (possibly) quarantine. See also: Public health; Vaccination





