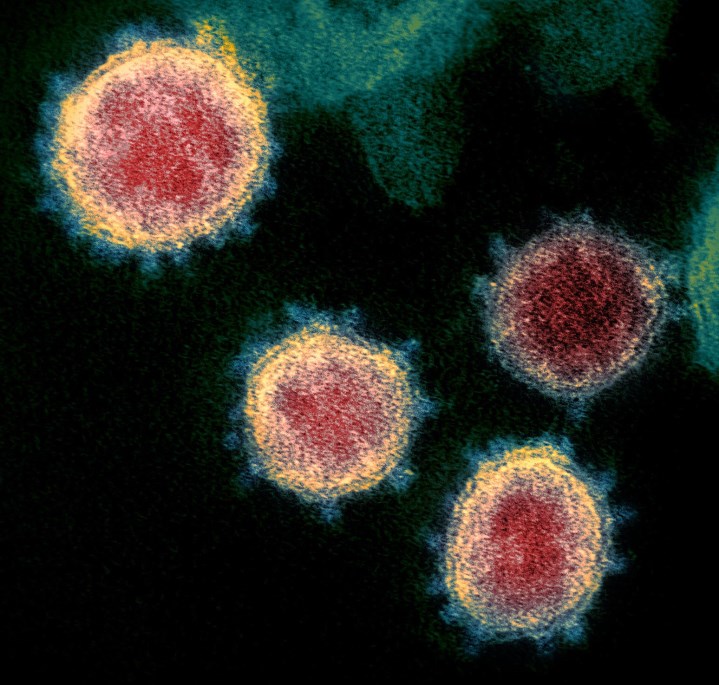
In response to the COVID-19 (coronavirus disease 2019) pandemic—which has dramatically affected the entire world, causing high morbidity, mortality, and massive social and economic disruption—and in addition to finding efficacious treatments for individuals severely affected by COVID-19, the global scientific community is focused on developing a safe and effective vaccine (or a number of different vaccines) to halt the pathogenic effects of the specific coronavirus—severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—that causes COVID-19 in humans. The potentially rapid development of a COVID-19 vaccine would reduce the degree and risk of infection, thereby decreasing transmission rates and ultimately controlling and ending the pandemic. However, some researchers are cautious about such a swift vaccine development because histories of past vaccine discoveries indicate that the process of creating a safe and effective vaccine is arduous, encompassing many years of research and clinical trials. Moreover, certain diseases have eluded efforts by scientists to find an effective vaccine. For example, there is as yet no vaccine to combat human immunodeficiency virus [HIV, the retrovirus that causes acquired immune deficiency syndrome (AIDS)], despite decades of research to develop such a vaccine. See also: Acquired immune deficiency syndrome (AIDS); Coronavirus; Epidemic; Human immunodeficiency virus (HIV); Immunology; Infection; Novel coronavirus is declared a global pandemic; Pathogen; Vaccination
The goal of vaccination is to immunize individuals against an infectious microorganism (or its components), thereby protecting the host against subsequent challenge by the infectious agent. Specifically, vaccines trigger an immune response against a particle or cell contained within the vaccine, which then leads to an "immunological memory" within the body and long-term protection against the target pathogen. The process of vaccine development is conducted incrementally, utilizing steps or stages involving potential vaccine identification, preclinical work, and, typically, three phases of clinical trials. If the vaccine is deemed successful, regulatory and governmental review and approval are mandated. The final stage of manufacturing astronomically large numbers of vaccine doses also requires a great deal of quality-control testing, so the total elapsed time from start to finish of vaccine development is never brief. For example, the shortest amount of time-to-market occurred in the case of the mumps vaccine, which required four years (in the 1960s) for the vaccine to be developed, approved, and marketed for use. See also: Biologicals; Clinical immunology; Immunity; Mumps; Production lead time; Quality control
Numerous pharmaceutical companies, scientific institutions, and government agencies in the United States, China, and multiple European countries began research efforts in early 2020 to identify COVID-19 vaccine prospects. Preliminary evidence indicates that individuals infected with SARS-CoV-2 produce antibodies, which are proteins in blood that neutralize viruses. Moreover, because scientists in China determined the genomic sequence of SARS-CoV-2 in January 2020, certain vaccine efforts are concentrating on genomic methodologies, particularly those involving DNA or messenger RNA (mRNA). For example, a promising mRNA vaccine candidate (mRNA-1273) has been developed by Moderna in Cambridge, Massachusetts. The first clinical batch of mRNA-1273 was completed in early February 2020. Importantly, researchers detected antibody production in the initial study group that received the potential vaccine, and levels of those neutralizing antibodies were high enough to confer immunity against COVID-19. No lingering side effects were noted as well. See also: Antibody; Cellular immunology; Deoxyribonucleic acid (DNA); DNA vaccination; Genetic mapping; Neutralizing antibody; Ribonucleic acid (RNA)
In mid-November 2020, Moderna announced that its mRNA vaccine had a 94.5% effectiveness rate against SARS-CoV-2. In addition, another fast-tracked mRNA vaccine developed jointly by Pfizer in the United States and BioNTech in Germany had an effectiveness rate of more than 95% in preventing COVID-19. No safety concerns were noted as well. In December 2020, the United Kingdom, the European Union, and the United States granted emergency use authorization to the Pfizer/BioNTech vaccine; this vaccine received full approval for use in the United States in late August 2021. The Moderna vaccine also was approved for emergency use in the United States.
Other research efforts are targeting the molecular structure of SARS-CoV-2 in attempts to pinpoint a vaccine. For example, spike (S) proteins, which protrude from the coronavirus's surface, are responsible for attaching the virus to a receptor present on the surface of a host cell. Most importantly, S proteins mediate fusion of the coronavirus with host cell membranes, allowing entry of the virus into the host cell. As such, S proteins are the main targets for antibodies produced by the body as an immune defense against the coronavirus. Thus, if binding of S proteins to host cell receptors could be blocked, as would be the case with an effective vaccine, the virus would not be able to enter the host cell. In particular, a vaccine (named ChAdOx1 nCoV-19) developed at the University of Oxford in coordination with AstraZeneca has shown positive results, with antibodies and T cells (T lymphocytes) being triggered to fight SARS-CoV-2 in individuals who received the vaccine. Excellent effectiveness (greater than 85%) and safety of the AstraZeneca/Oxford University vaccine from phase-III trials were reported in early December 2020, and the vaccine was approved for emergency use in the United Kingdom and the European Union in late December 2020 and late January 2021, respectively. See also: Cell membrane; Protein; Virus
Moreover, in late January 2021, a vaccine with an effectiveness of 85% in preventing severe disease in patients, and 100% effective in preventing hospitalization and death in patients, was announced by Johnson & Johnson in the United States. This vaccine was approved for emergency use in the United States in late February 2021.
Ad5-nCoV, an engineered adenoviral-vector vaccine that contains adenovirus type 5 (a common cold virus), is a promising vaccine candidate that impedes S protein binding. When the vaccine is deployed into a host and recognized by the host’s immune system, neutralizing antibodies against the S proteins of SARS-CoV-2 are produced. Ad5-nCoV was developed by CanSino Biologics in China, and phase-II trials were completed in August 2020. The results of this vaccine have been positive in more than 100 human test subjects, who have been assessed with regard to both the safety of the vaccine and its ability to generate a successful immune response. See also: Adenoviridae
Another prototype vaccine, Ad26, which is a chemically disabled version of an adenovirus that has been engineered to contain a gene for the S proteins of SARS-CoV-2, has tested successfully in eight rhesus monkeys. The Ad26 vaccine was created by researchers at Beth Israel Deaconess Medical Center and Harvard Medical School in Boston, Massachusetts, in March 2020, with positive results being reported since then. Deployment of this vaccine caused the monkeys to produce neutralizing antibodies against SARS-CoV-2. However, monkeys typically fail to develop the most severe symptoms that SARS-CoV-2 causes in humans, so it is unknown whether humans would develop similar immunity to the coronavirus as the monkeys did in response to the vaccine. Still, the ability of a vaccine to work efficaciously in an animal model is a hopeful sign that such a vaccine may work in humans. See also: Animal testing
Notably, various SARS-CoV-2 mutations have appeared as well, which may be more transmissible. For example, mutant strains of the coronavirus in India, South Africa, Brazil, and the United Kingdom are being evaluated and tracked closely by epidemiologists because these strains have been detected in other locations around the world. In particular, the mutant Delta variant (B.1.617.2, which originated in India) is highly contagious, being especially transmissible among unvaccinated individuals. So far, the approved vaccines have shown protection against the variants.
Numerous research teams continue to work on development of other safe and effective COVID-19 vaccines.





